Obsessive Compulsive Disorder (OCD)
Table of Contents for OCD
-
Clinical Pathways and Rating Scales
-
Rating Scales
-
Assessment and Diagnosis
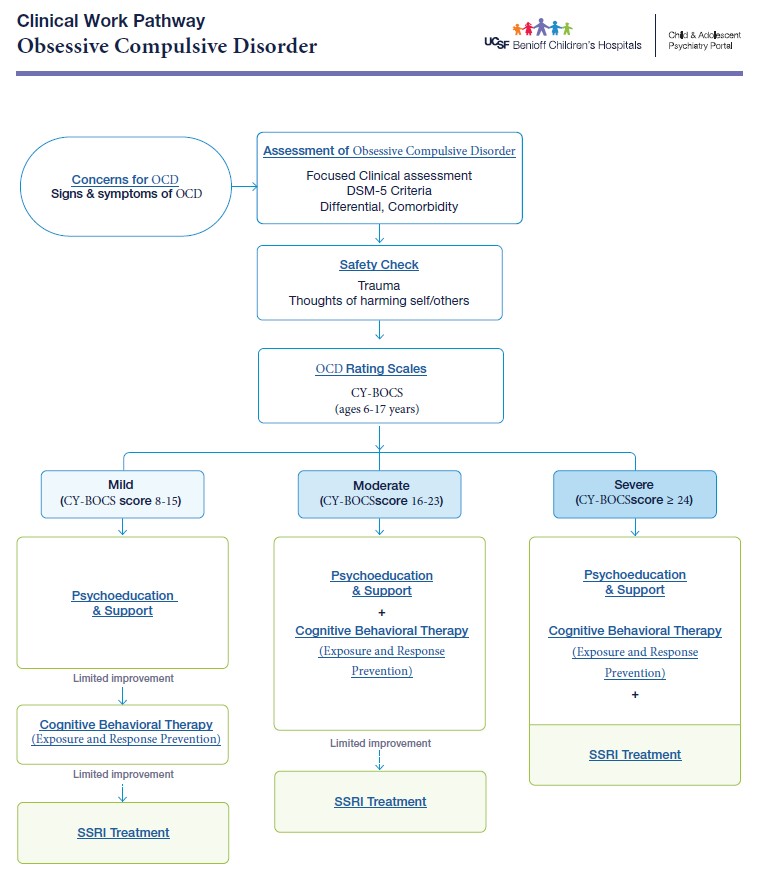
Clinical Pathway and Rating Scales for OCD
***Download Full PDF***
CY-BOCS (Child Yale-Brown Obsessive Compulsive Scale)
- Ages: 6-17 years
- Not a screening tool but used as a rating scale to characterize and track symptoms.
- Used in the Comprehensive Diagnostic process of OCD, track symptom progress
- Symptom checklist - Past, Current symptoms
- Severity rating scale - Mild, Moderate, Severe
|
Common Signs and symptoms of OCD |
|
Irritability, Anger, Temper tantrums Worries or Intrusive Thoughts (Obsessions)
Habits or Rituals (Compulsions)
Excessive and time-consuming Interferes with social, family, school functioning. |
|
DSM-5 Criteria for Obsessive Compulsive Disorder (OCD) |
|
|
Obsessions |
“WORRIES,” recurrent thoughts, urges, or images experienced as intrusive or unwanted and cause distress/anxiety leading to an attempt to ignore, suppress, or neutralize them with another thought or action (compulsion) |
|
Compulsions |
“RITUALS OR HABITS,” behaviors that feel necessary in response to an obsession or according to rules that must be applied rigidly to reduce anxiety/distress or prevent a feared event or situation. However, the behaviors may or may not be connected to what they are designed to neutralize or are clearly excessive. |
|
|
Focused Clinical Assessment (Clinical Pearls for History Taking)
|
Focused clinical history |
|
|
Collateral history |
|
|
Assess for functioning in multiple domains |
|
|
Assess for acute stressors |
|
|
Assess for Trauma history, chronic stress |
|
|
Longitudinal clinical hx of symptoms |
|
|
Differential diagnosis
|
|
|
Comorbidities
|
Highly comorbid with childhood OCD
|
****Needs Feedback/Update****
Psychoeducation
- Avoidance is one of the key parts of anxiety and OCD symptoms. When something makes us anxious, we tend to avoid it (flight response) or engage in maladaptive behaviors (rituals, habits) which then temporarily relieves the anxiety. However, most of the things that we worry about we can’t avoid forever, and the more we avoid or engage in maladaptive behaviors to lessen the anxiety the bigger and stronger the anxiety, maladaptive habits get. Like in the studying procrastination example, the longer you put off studying for a test, the more the anxiety builds. This creates a feedback loop where the more anxious someone is, the more they avoid, or engage in a maladaptive behavior and the bigger the anxiety gets.
- Exposures are a strategy for stopping this feedback loop. Exposures are the opposite of avoidance; you expose yourself to what’s making you anxious instead of avoiding it. While this increases your anxiety short term, with continued exposures your anxiety goes down. This is due to a process called habituation where your body gets used to things over time. Exposures are approached in a step-wise manner; you start by exposing yourself to something that’s a little anxiety-provoking and practice tolerating that. Once that’s okay, you gradually practice exposures to medium and then very anxiety-provoking things. For instance, if someone is afraid of snakes, they might start by talking about snakes, then looking at pictures, then a video, gradually working up to managing their anxiety while seeing a live snake.
Parent and School Supports
- Psychoeducation to destigmatize and reframe presenting symptoms is important because children are often secretive about their OCD symptoms, so they may be misinterpreted.
- Work with parents and schools to gradually decrease ways they are accommodating for and reinforcing OCD symptoms.
Psychotherapy
Exposure and Response Prevention Therapy (ERP)
- Exposure and Response Prevention (ERP) is a form of Cognitive Behavioral Therapy (CBT) in treating Obsessive Compulsive Disorders (OCD).
- ERP is time-limited therapy, usually 12-20 sessions, involving both the child and family.
- The patient is gradually exposed to their fears in a controlled setting and learns how to resist the compulsion.
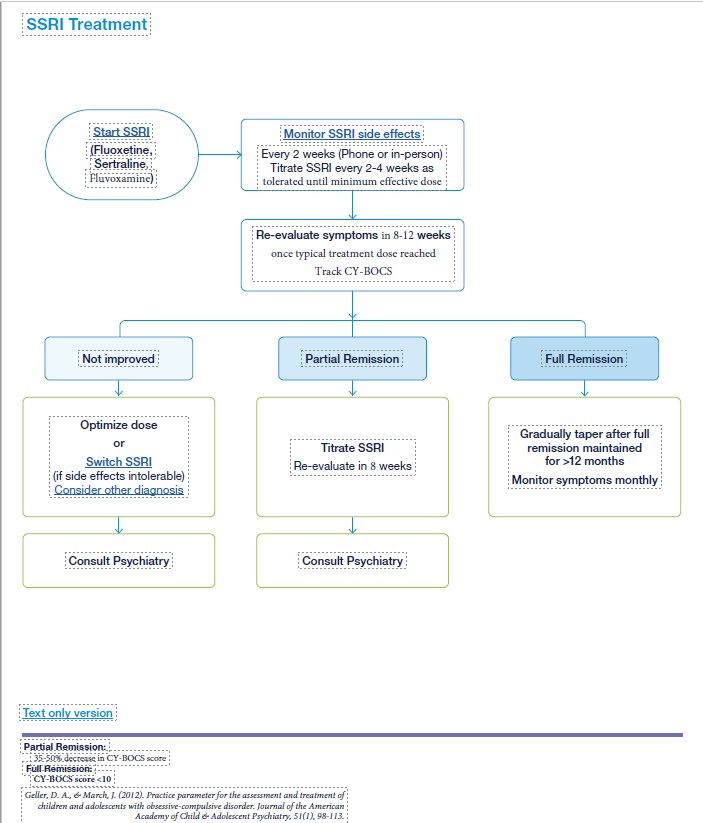
- First-line recommended medication: Selective Serotonin Reuptake Inhibitor (Fluoxetine, Sertraline, Fluvoxamine)
- Indications
- Severe OCD (CY-BOCS scores 24 and above)
- Limited improvement with therapy in moderate OCD (CY-BOCS scores 16-23)
- OCD symptoms interfering with ability to engage in therapy, exposures.
- SSRI treatment response may take 8-12 weeks at adequate treatment dose
- If symptoms do not improve, switch to different SSRI.
- May consider SSRI gradual taper after atleast >12 months of maintaining remission status to prevent relapse.
- SSRI treatment algorithm ***needs update ***
- SSRI Dosing Guidelines for OCD **Edit Table with Design Team***
-
FDA approved
Drug
Starting Dose (mg)
Typical Dose Range (mg)
(Mean dose)
Pre-adolescent
Adolescent
Sertraline (Zoloft)
12.5 - 25
25-50
50-200 (178)
Fluoxetine (Prozac)
2.5 - 10
10-20
10-80 (25)
Fluvoxamine(Luvox)
12.5-25
25-50
50-300 (165)
Adapted from Practice parameter for the assessment and treatment of children and adolescents with obsessive-compulsive disorder. (2012). Journal of the American Academy of Child and Adolescent Psychiatry, 51(1), 98–113. https://doi-org.ucsf.idm.oclc.org/10.1016/j.jaac.2011.09.019
PCP Tipsheets ***needs upload/update
SSRI Tipsheet for Primary Care Providers (PDF) ***Edit and adpat to OCD Guidelines***
Switching SSRIs (PDF) ***update? include?***
Clinical Pathway ***needs update
OCD Clinical Pathway (PDF) *** needs Design team/update***
Online Resources
Family Resources for OCD
Handouts***update needed**
- OCD Book Recommendations (PDF) ***needs update***
Online Resources *** update needed
Book Recommendations***need to update/keep vs delete***
Book Recommendations:
- For parents:
- Freeing Your Child from Obsessive-Compulsive Disorder: A Powerful, Practical Program for Parents of Children and Adolescents by Tamar E. Chansky, PhD
- For teens:
- Talking Back to OCD: The Program That Helps Kids and Teens Say "No Way" -- and Parents Say "Way to Go" by John S. March, MD
- For younger kids (to read together with parents):
- Up and Down the Worry Hill: A Children's Book about Obsessive-Compulsive Disorder and its Treatment by Aureen Pinto Wagner, PhD and illustrated by Paul A. Jutton
- What to Do When Your Brain Gets Stuck: A Kid's Guide to Overcoming OCD by Dawn Hubner, PhD and illustrated by Bonnie Matthews
Contact Us
Phone: 800-253-2103
To Request a Consult:
Step 1: Register Here for your Cal-MAP account
Step 2: Create your new password.
Step 3: Request your first consultation!
-
Cal-MAP Office Hours Monday - Friday 8:30am-4:30pm
For technical assistance, reach our support team via phone, chat or email request.
