-
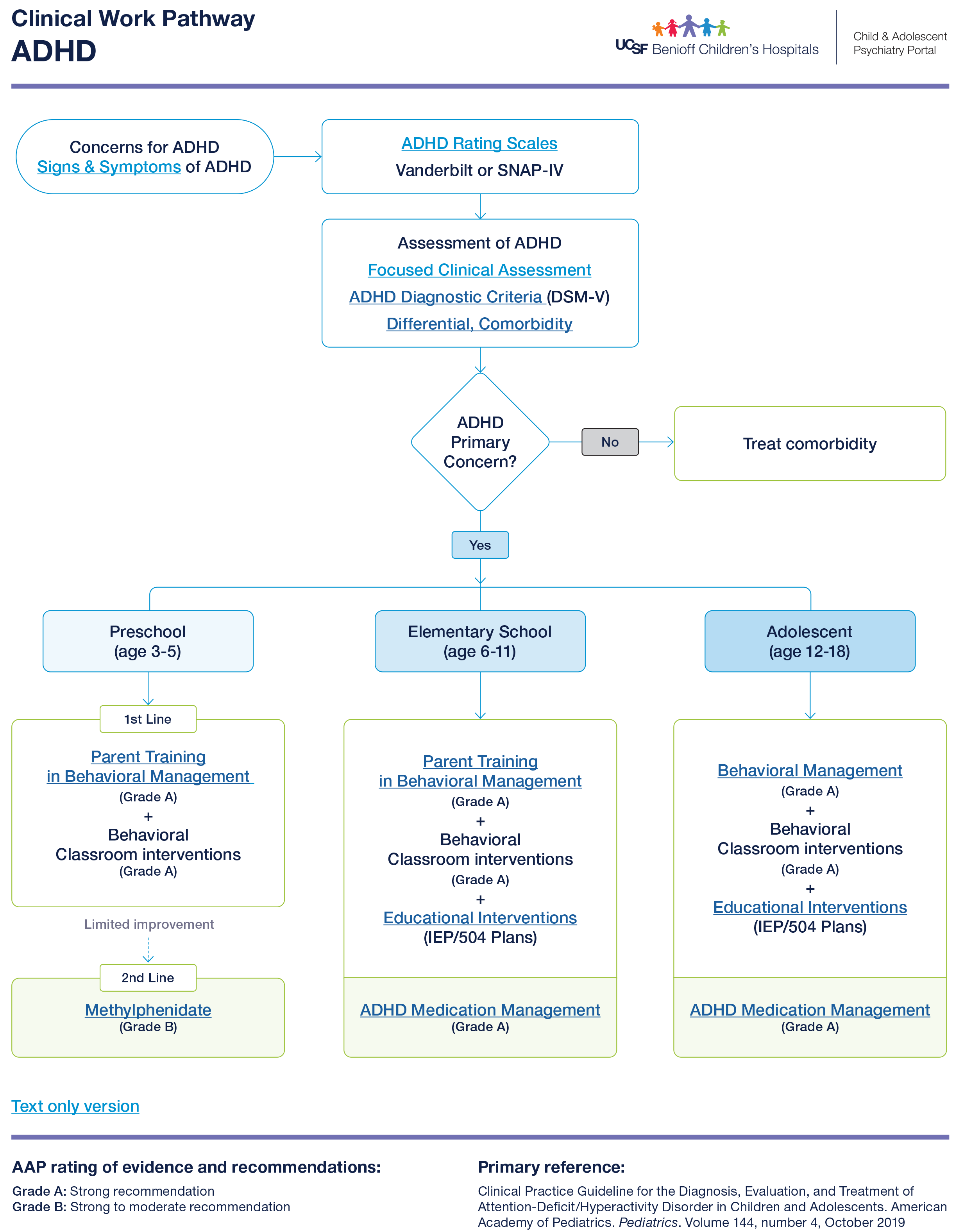
Vanderbilt (ages 6-12 years)
-
SNAP-IV (Swanson, Nolan and Pelham Teacher and Parent rating scale, ages 6-18 years)
-
ASRS-V1.1 (Adult ADHD Self-Report Scale): English
PCIT
PCIT is an evidence-based treatment (EBT) for preschool aged children with disruptive behavioral problems. It is conducted through “coaching” sessions where a therapist observes through a one-way mirror while the parent and child is observed interacting in the playroom. The therapist will be coaching you live on how to manage your child’s behaviors from outside the one-way mirror observing you and directing the parent through a “bug-in-the-ear” device.
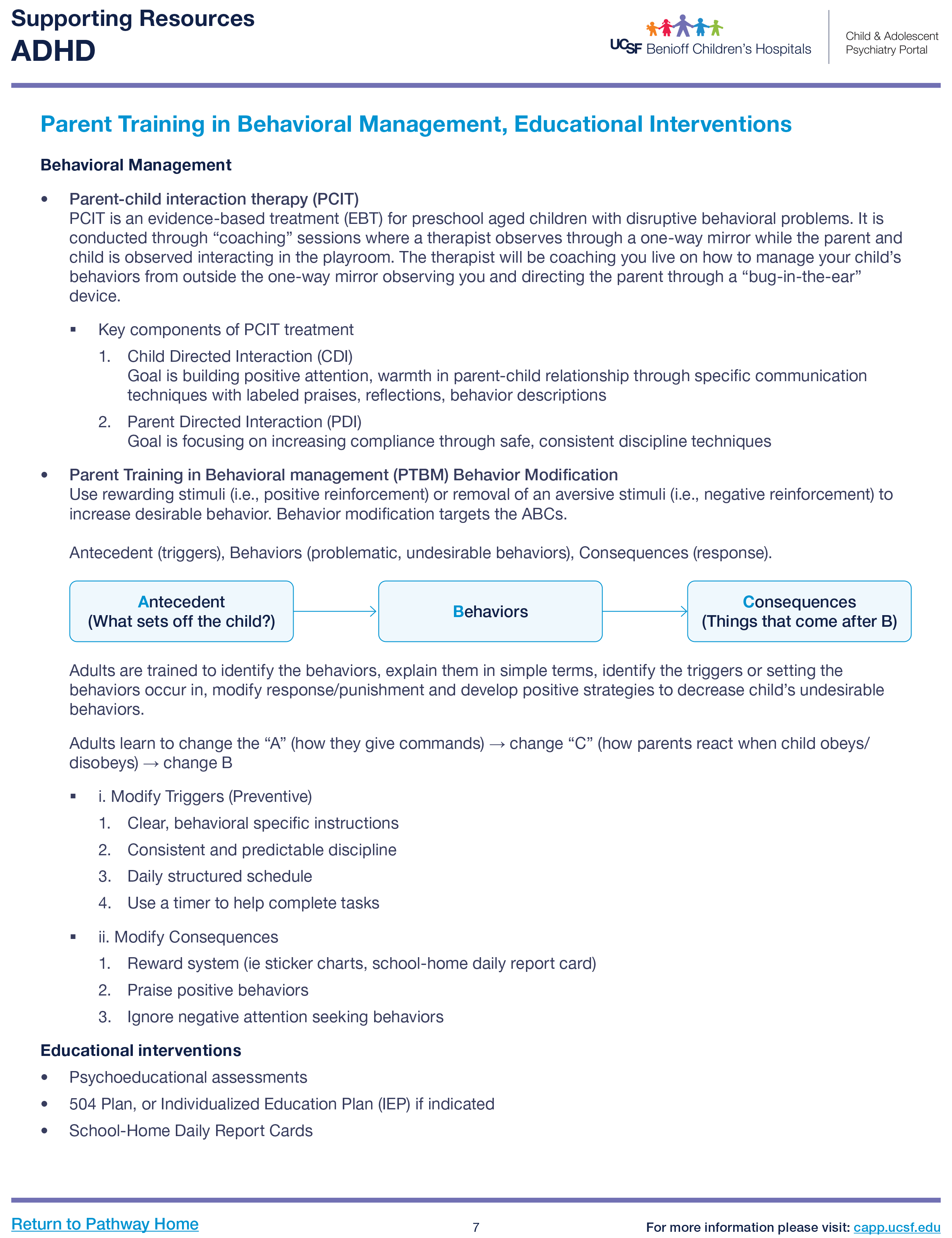
Parent Training in Behavioral Management (PTBM)
Use rewarding stimuli (i.e., positive reinforcement) or removal of an aversive stimuli (i.e., negative reinforcement) to increase desirable behavior.
Adults are trained to identify the behaviors, explain them in simple terms, identify the triggers or setting the behaviors occur in, modify response/punishment, and develop positive strategies to decrease child’s undesirable behaviors.
Modify Triggers (Preventive)
Clear, behavioral specific instructions
Consistent and predictable discipline
Daily structured schedule
Use a timer to help complete tasks
Modify Consequences
Reward system (ie. sticker charts, school-home daily report card)
Praise positive behaviors
Ignore negative attention seeking behaviors
-
Psychoeducational assessments
-
504 Plan, or Individualized Education Plan (IEP) if indicated.
Clinical Pathway for ADHD
NICHQ ADHD Toolkit
Special Education Resources
DREDF (Disability Rights Education and Defense Fund)
Handouts
NICHQ ADHD Toolkit
Special Education Resources
DREDF (Disability Rights Education and Defense Fund)
Click here for resource: Parents’ Medication Guide for ADHD
Children and Adults with ADHD (CHADD)
Click here for resource: Understood
-
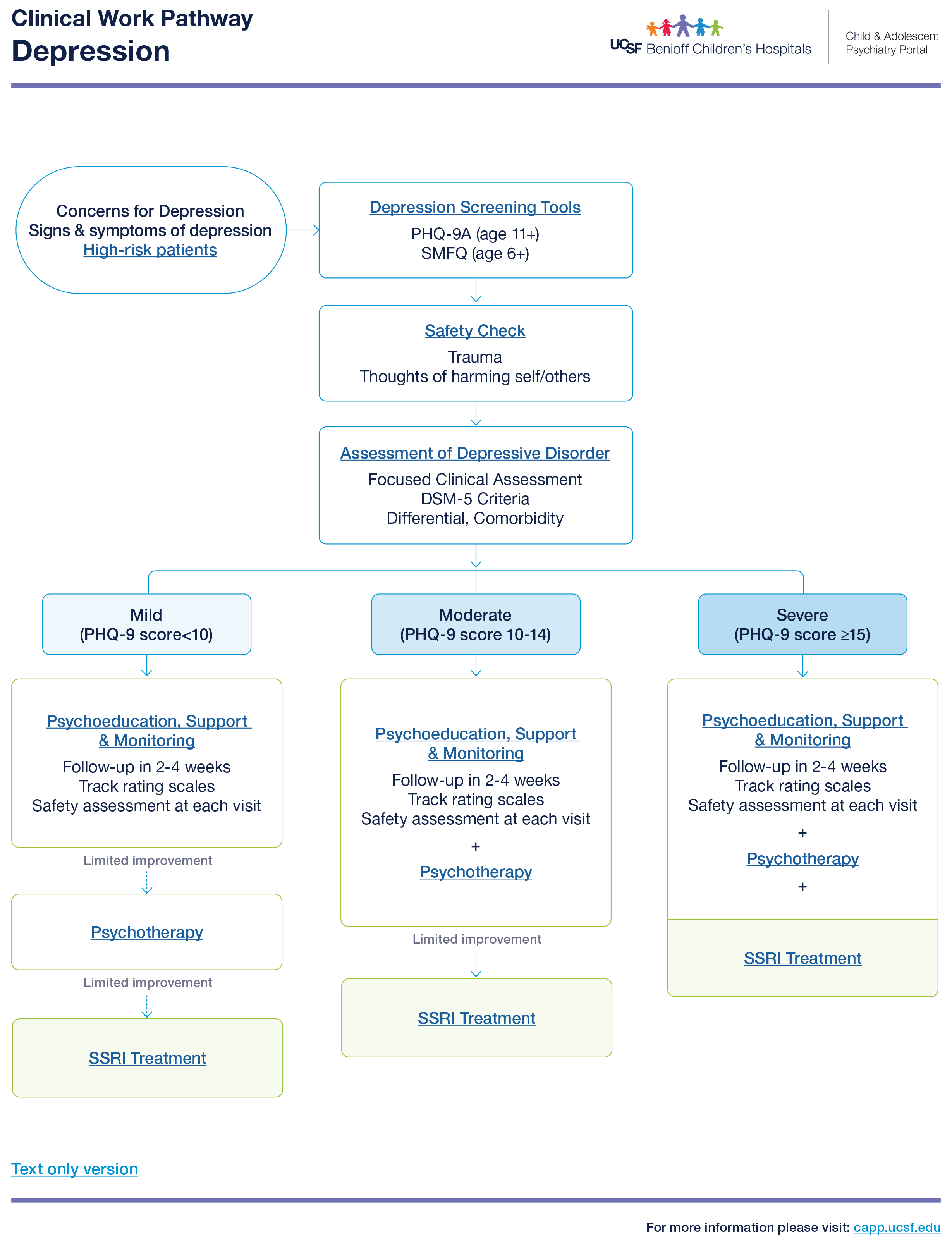
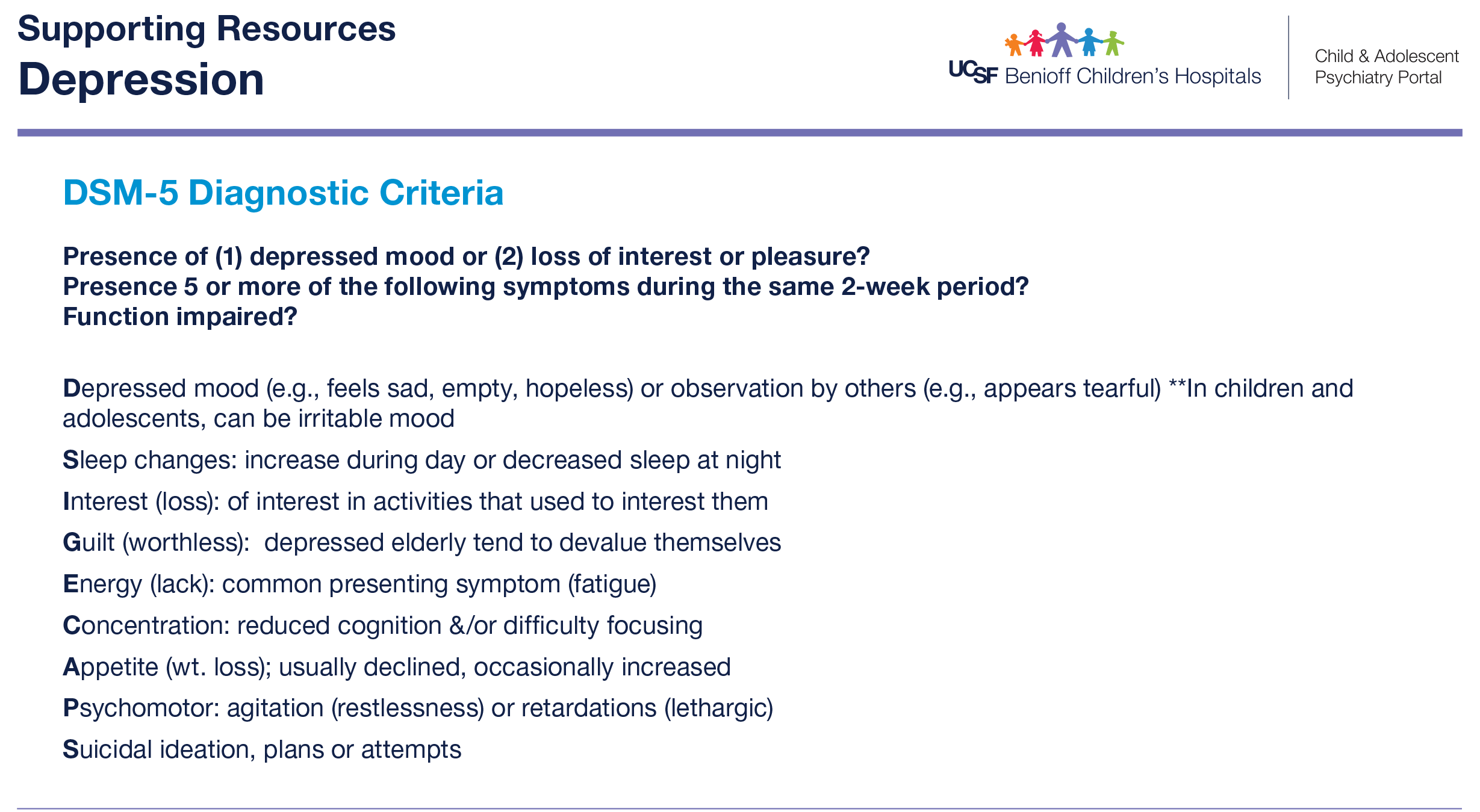
Rule out Depression – PHQ-9
-
If any obsessions/compulsions – rule out OCD – CY-BOCS
-
If any trauma hx, nightmares/flashbacks – rule out PTSD
Psychoeducation

-
Normalization
-
Anxiety is a normal part of life. Everyone experiences anxiety sometimes, but it can become a problem if it’s causing you a lot of distress or getting in the way of your functioning. Our brains use the fight, flight, or freeze response to help us stay safe. Have you heard of this before? Basically, it means that when our brains perceive a threat, we often respond by fighting (arguing, irritability), fleeing (avoidance), or freezing (shutting down). While a little anxiety can be helpful, too much can get in the way of things. For instance, a little anxiety might help motivate you to study for your test, but too much anxiety can lead to procrastination (avoidance) which while in the short term may make you feel better, isn’t helpful in the long term.
-
-
Education on Avoidance
-
Avoidance is one of the key parts of anxiety. When something makes us anxious, we tend to avoid it (flight response) which then temporarily relieves the anxiety. However, most of the things that we worry about we can’t avoid forever, and the more we avoid something the bigger the anxiety gets. Like in the studying procrastination example, the longer you put off studying for a test, the more the anxiety builds. This creates a feedback loop where the more anxious someone is, the more they avoid, and the bigger the anxiety gets.
-
Exposures are a strategy for stopping this feedback loop. Exposures are the opposite of avoidance; you expose yourself to what’s making you anxious instead of avoiding it. While this increases your anxiety short term, with continued exposures your anxiety goes down. This is due to a process called habituation where your body gets used to things over time. Exposures are approached in a stepwise manner; you start by exposing yourself to something that’s a little anxiety-provoking and practice tolerating that. Once that’s okay, you gradually practice exposures to medium and then very anxiety-provoking things. For instance, if someone is afraid of snakes, they might start by talking about snakes, then looking at pictures, then a video, gradually working up to managing their anxiety while seeing a live snake. If your anxiety is milder, you can practice exposures at home with the support of your family and written resources. If your anxiety is more severe, you can work with a therapist to practice exposures as part of a treatment called Cognitive Behavioral Therapy (CBT).
-
Relaxation Technique
Strategies to calm down the body’s fight or flight response and reduce anxiety.
Deep breathing
1. Belly breathing
-
Sit comfortably with hands on belly.
-
Breath in slowly through your nose.
-
Imagine you are blowing up a balloon that is expanding against your hand.
-
Breathe out slowly through your mouth, deflating the balloon.
-
Try to make your exhale longer than your inhale.
2. 3-4-5 breathing
-
Inhale for 3 counts
-
Hold for 4 counts.
-
Exhale for 5 counts
3. Fun ways to practice breath control: pinwheels, blowing bubbles, whistling.
Muscle Relaxation: tensing muscles and then releasing them allows them to relax.
Robot Ragdoll
-
First try to be stiff like a robot, keep your muscles tight.
-
Then relax all your muscles, try to be floppy like a ragdoll.
Progressive muscle relaxation (PMR)
-
Sequentially tense then relax each muscle group.
-
Start by curling your toes tight for 5 seconds then release.
-
Then tense your calves for 5 seconds then release.
-
Gradually move up to the head.
-
Analogies, such as shrugging your shoulders like a turtle, can be helpful for younger children.
Imagery
-
Think of a place that is calming for you.
-
Imagine every detail, including each sense (sights, sounds, smell, taste, feel)
Mantra – A phrase to help calm and refocus.
-
Think of a coping thought.
-
Practice repeating this phrase when you’re anxious.
-
Examples: “This too shall pass”, “I am enough”, “I can control my panic with breathing”
Cognitive Behavioral Therapy (CBT)
 CBT is a type of time-limited therapy based on the concept that thoughts, behaviors, and feelings all affect each other and that by changing our thoughts and behaviors, we can change how we feel. It is often the first choice for children and teens with depression, which ranges from 6-20 sessions. It is the psychotherapy with the most evidence for treatment of childhood anxiety disorders. It consists of five main parts:
CBT is a type of time-limited therapy based on the concept that thoughts, behaviors, and feelings all affect each other and that by changing our thoughts and behaviors, we can change how we feel. It is often the first choice for children and teens with depression, which ranges from 6-20 sessions. It is the psychotherapy with the most evidence for treatment of childhood anxiety disorders. It consists of five main parts:
1. Psychoeducation to both child and parent about anxiety disorders and CBT
2. Somatic management skills training
3. Cognitive restructuring
4. Exposures
5. Relapse prevention plans
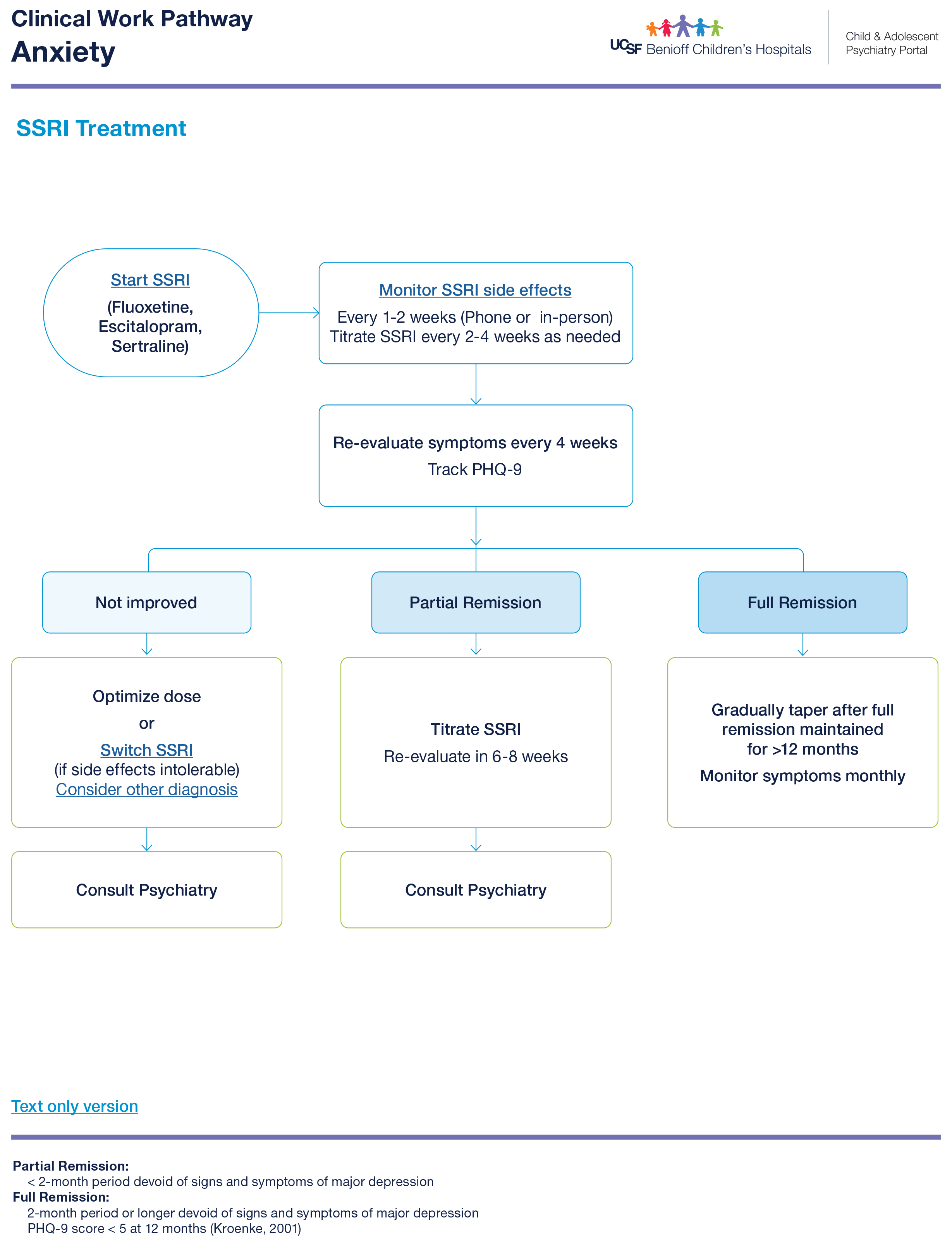
First-line recommended medication: SSRI (Fluoxetine, Sertraline)
Indications
-
Limited improvement with therapy
-
Anxiety interfering with ability to engage in therapy, exposures.
-
Severe Anxiety (GAD-7 > 16)
-
Comorbid disorder requires treatment.
-
Continue SSRI for at least 6 months into remission before considering weaning off medication.
-
SSRI treatment flow chart
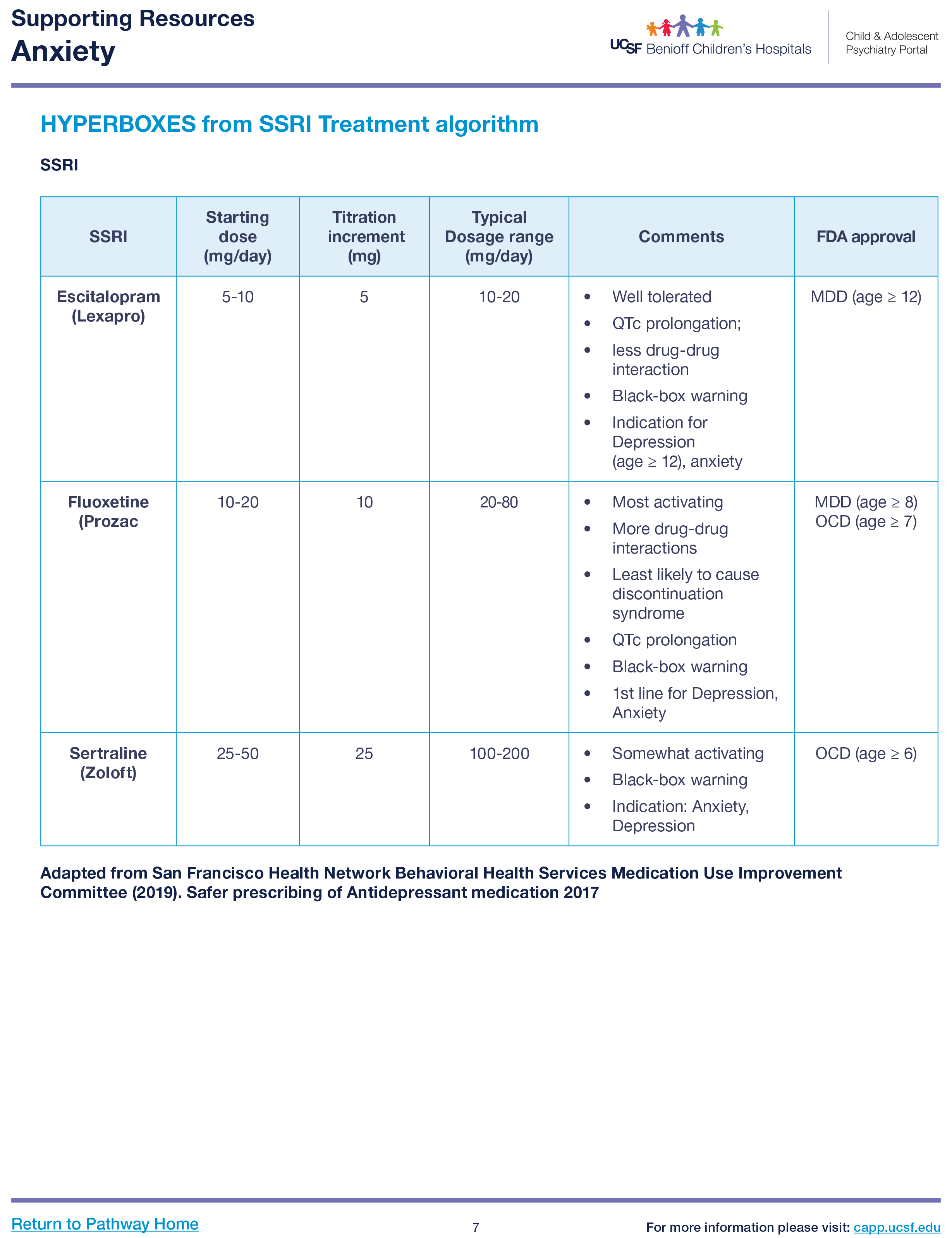
SSRI
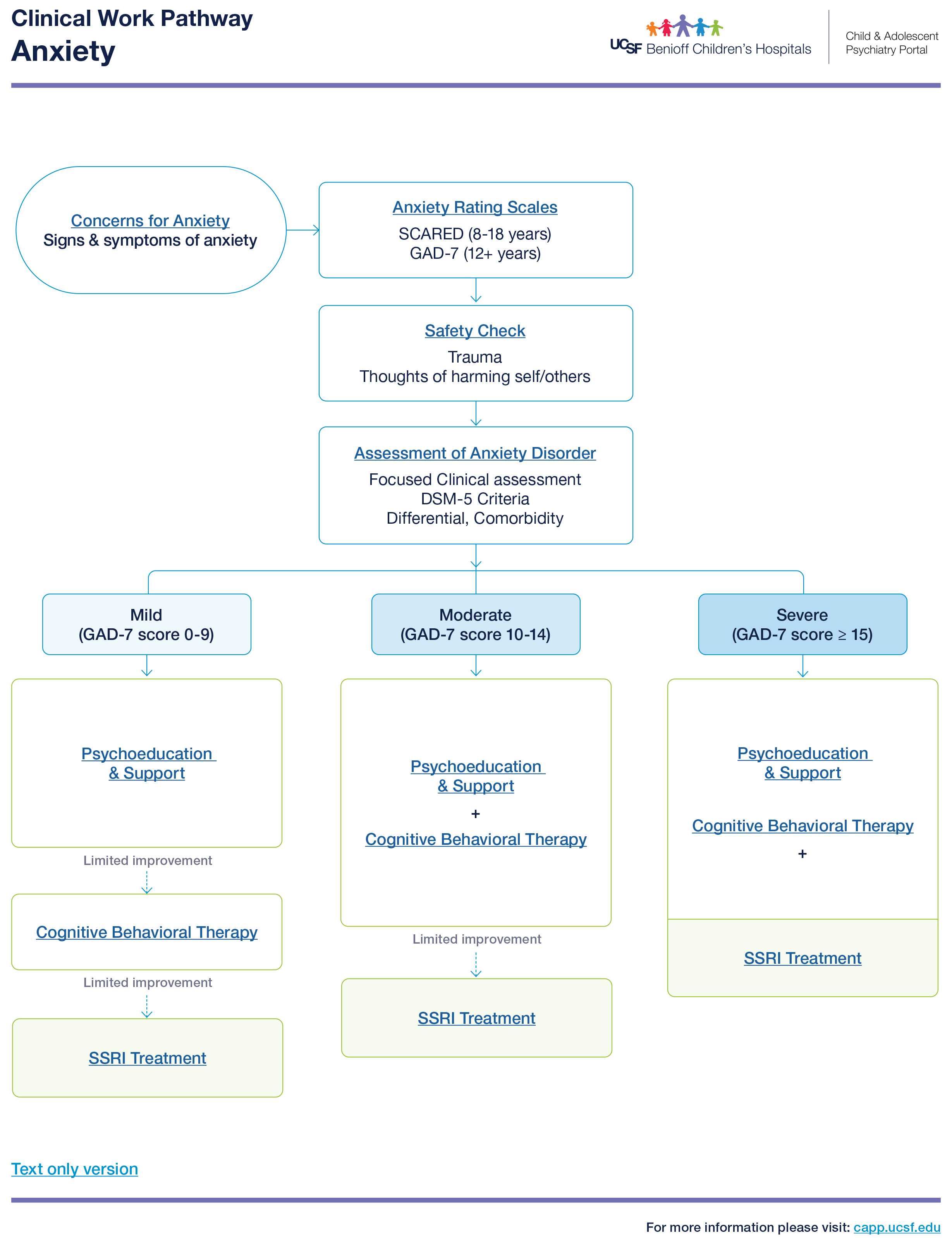
Clinical Pathway for Anxiety
Handouts
Click here for resource: Anxiety Book Resources
Online Resources
Click here for resource: Tools for supporting Emotional Wellbeing in Children and Youth
Click here for resource: AACAP Anxiety Disorders Resource Center
Click here for resource: Anxiety & Depression Association America
Click here for resource: Anxiety Canada
Click here for resource: The National Child Traumatic Stress Network
Click here for resource: Coping Cat Parents
-
Short Moods and Feelings Questionnaire (SMFQ, ages 6-19 years): Child Report | Parent Report | Scoring
-
CES-DC (Center for Epidemiological Studies – Depression scale for children, ages 6-17 years): English
-
EDPS (Edinburgh Postpartum Depression Scale) English | Spanish
-
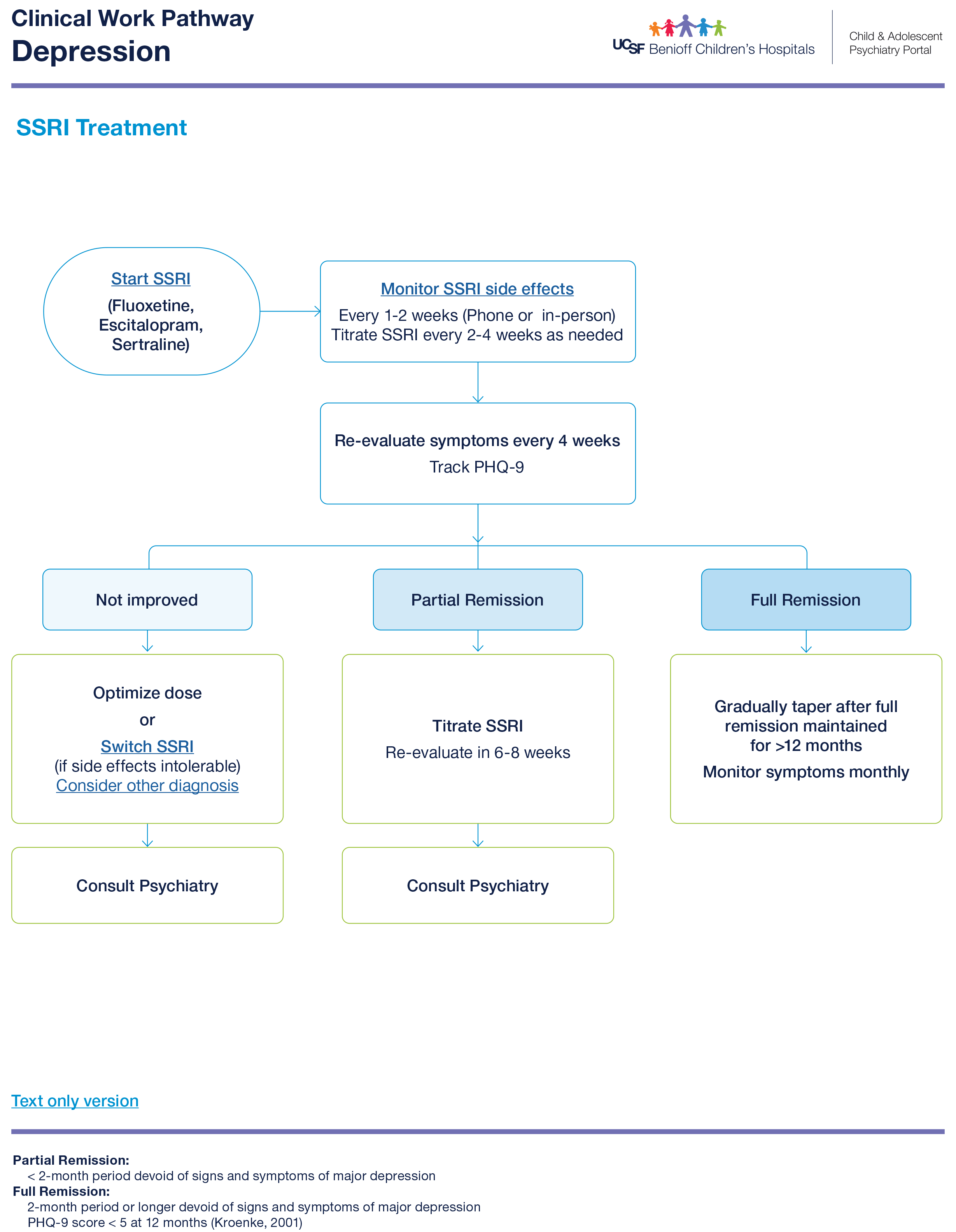
First-line recommended medication: SSRI (Fluoxetine, Escitalopram, Sertraline)
-
Indications (can be fold out? If too lengthy)
-
Limited improvement with therapy
-
Depression interfering with ability to engage in therapy, exposures.
-
Severe Depression (PHQ-9 ≥ 15)
-
Comorbid disorder requires treatment.
-
-
Continue SSRI for at least 9-12 months into remission before considering weaning off medication.
-
SSRI treatment flow chart
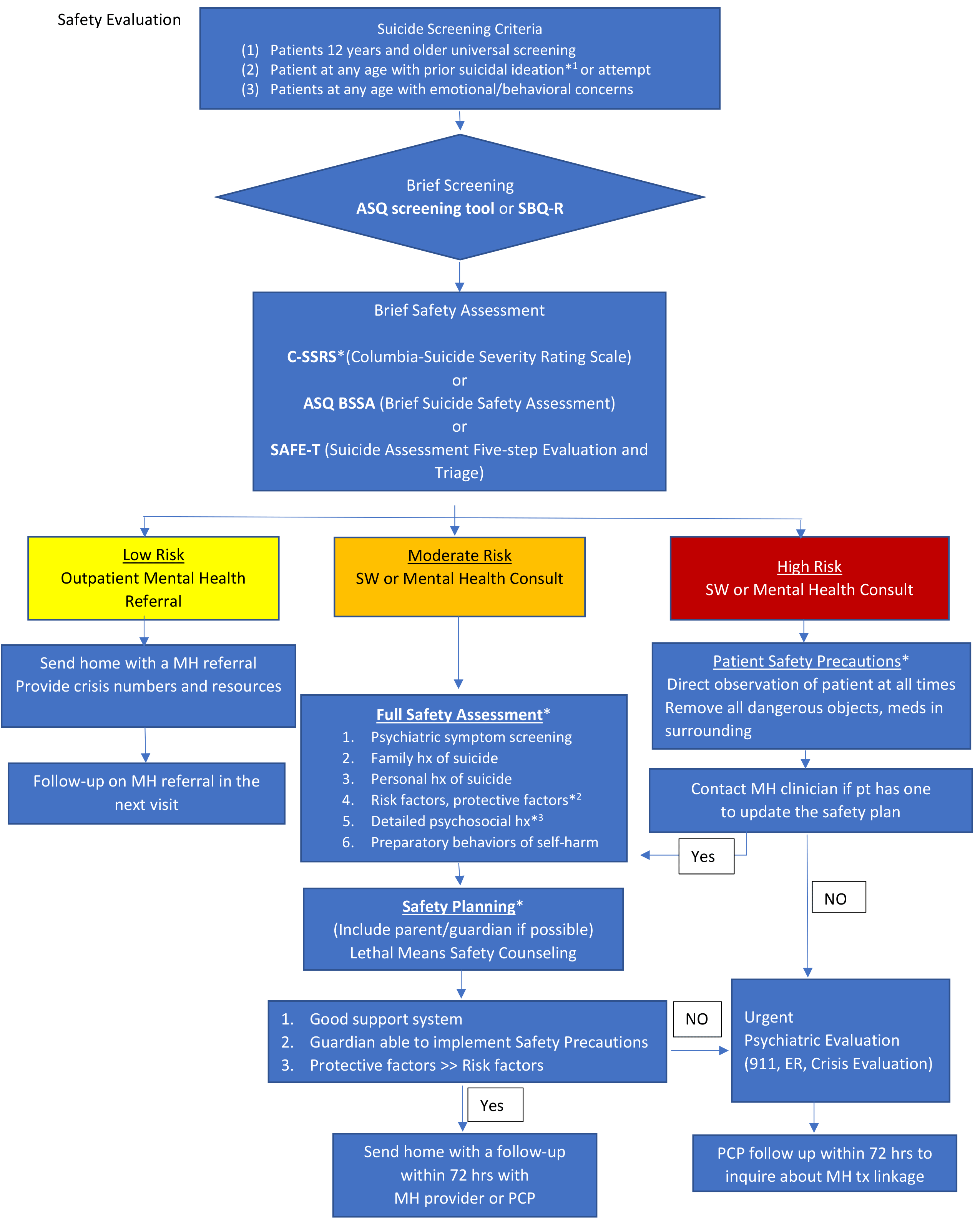
Click here for resource: Suicide and Safety
AAP Endorsements – Guidelines for Adolescent Depression in Primary Care (GLAD-PC)
Handouts
Suicide Prevention: A Resource for Parents and Caregivers – AAP (PDF)
Click here for resource: (PDF)
Click here for resource: Emotion Coping Skills Resources
Online Resources
Click here for resource: Tools for supporting Emotional Wellbeing in Children and Youth
Click here for resource: AACAP Depression Resource Center
Click here for resource: AACAP Suicide Resource Center
Teen Suicide Prevention – Mayo Clinic (Video)
Click here for resource: Anxiety & Depression Association America
Click here for resource: Families for Depression Awareness
Click here for resource: National Alliance on Mental Illness (NAMI)
Effective Child Therapy (Evidence-based Mental Health Therapy for children and adolescents)
Click here for resource: Effective Child Therapy
Click here for resource: The National Child Traumatic Stress Network
Click here for resource: StopBullying.gov
Crisis Resources
National Suicide Prevention Lifeline 988 Suicide & Crisis Lifeline (Call, Chat, or Text 988)
Click here for resource: 988 Suicide & Crisis Lifeline (Call, Chat, or Text 988)
Crisis Text Line (Text HOME to 747747)
Click here for resource: Crisis Text Line (Text HOME to 747747)
Click here for resource: The Trevor Project
Together with patient: NIMH ASQ BSSA (Brief Suicide Safety Assessment) Worksheet
Enter content.
For Provider (reference): BSSA Provider Guide
Enter content.
Good evidence supporting use of Safety Planning and Lethal Means reduction to reduce suicide attempts and completed suicides.
Link to resource: Handout for Family
AAP Clinical Report: Suicide and Suicide Attempts in Adolescents (Article)
Link to resource: (Article)
Online Resources
American Academy of Pediatrics (AAP)- Suicide: Blueprint for Youth Suicide Prevention
Enter content.
Getting Help
National Suicide Prevention Lifeline 988 Suicide & Crisis Lifeline (Call, Chat, or Text 988)
Enter content.
Crisis Text Line (Text HOME to 747747)
Enter content.
Enter content.
Handouts for Families
Online Resources

 Link to full PDF:
Link to full PDF: